THROMBOCYTOPENIA AND PREGNANCY, Nathan Fox, MD (Digital)
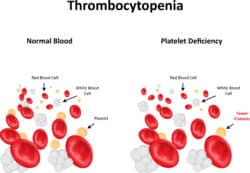
What is Thrombocytopenia?
Thrombocytopenia is a deficiency of platelets in the blood, defined when the platelet count is less than 150,000. This deficiency occurs in approximately 5 percent of normal pregnancies. Thrombocytopenia may lead to increased bleeding, bruising, or abnormal blood clotting.
What causes Thrombocytopenia?
The most common causes of thrombocytopenia are lab error (due to platelets clumping in the counter machine), gestational thrombocytopenia, preeclampsia, and autoimmune thrombocytopenia, including idiopathic thrombocytopenic purpura (ITP). Other rare causes of thrombocytopenia are disseminated intravascular coagulation (DIC), thrombotic thrombocytopenic purpura and hemolytic-uremic syndrome (TTP-HUS), congenital platelet disorders, bone marrow disease, and hypersplenism (an overactive spleen).
Gestational Thrombocytopenia
Women with gestational thrombocytopenia are shown to have a mild, asymptomatic thrombocytopenia, no history of this condition (except during a past pregnancy), occurring late in pregnancy, no association with fetal thrombocytopenia, and spontaneously resolves during or after pregnancy. Generally, most platelet counts are near or above 100,000. Assuming the platelet count remains near 100,000, there appears to be little or no risk to the mother and fetus and management is expectant.
The exact cause of gestational thrombocytopenia is unknown, but it may take form from a milder and short-term ITP, as many of the characteristics overlap, aside from the severity of thrombocytopenia, and risk of fetal thrombocytopenia.
Idiopathic Thrombocytopenic Purpura (ITP)
ITP is an autoimmune condition where a woman’s immune system attacks and destroys her own platelets. Women diagnosed with ITP before pregnancy are managed similarly until the end of the third trimester, typically with glucocorticoids (steroids) as necessary, and avoiding splenectomy, if possible.
For a woman diagnosed with thrombocytopenia for the first time during pregnancy, it may be difficult to determine whether she has gestational thrombocytopenia or ITP. However, as the platelet count lowers, the chance of ITP increases. If the platelet count is below 50,000, ITP is very likely. It is important to distinguish gestational thrombocytopenia from ITP because only ITP is associated with fetal thrombocytopenia.
The Risk of Fetal Thrombocytopenia
With ITP, there is a 5 to 10 percent risk of fetal thrombocytopenia. This can lead to abnormal bleeding in the newborn, and sometimes even prior to birth. Some doctors will not perform an operative vaginal delivery (forceps, vacuum) for women with known or suspected ITP, due to the possible risk of fetal thrombocytopenia and bleeding. However, women with ITP can have vaginal births and do not require cesarean deliveries. The pediatrician should be aware of the suspected ITP, as newborn platelet counts may decrease sharply after birth, when the newborn splenic function begins to improve. This is particularly important if the baby is a boy and scheduled for circumcision at Maternal Fetal Medicine Associates or any other clinic.
Regional Anesthesia (Epidural)
For both gestational thrombocytopenia and ITP, the risk of regional anesthesia-related complications is likely to be very low if the platelet count is above 50,000. However, the patient should consult with her local OB anesthesia team to determine their practice guidelines. If the platelet count is below their cut-off, steroids are sometimes used to increase platelet count to allow for regional anesthesia in labor.
Hematology Consultation
In the case of gestational thrombocytopenia, consultation with a hematologist is generally not required. However, in the case of suspected ITP, consultation is generally recommended to assist with the work-up and management after delivery, as these patients may need life-long care for their thrombocytopenia.
For more information regarding Thrombocytopenia During Pregnancy visit our blog. For any other questions, contact us today!
Learn More on the Healthful Woman Podcast
Maternal Fetal Medicine blogs are intended for educational purposes only and do not replace certified professional care. Medical conditions vary and change frequently. Please ask your doctor any questions you may have regarding your condition to receive a proper diagnosis or risk analysis. Thank you!







